District Comprehensive Communicable Disease Plan
COMPREHENSIVE COMMUNICABLE DISEASE MANAGEMENT PLAN
Updated: October 2, 2025
Adapted for MESD and its component districts (Reynolds School District) with permission from Dr. Jan Olson and team’s comprehensive communicable disease management plan for the Molalla River School District.
THIS PLAN CONTAINS:
RSD Communicable Disease Prevention Plan
RSD Exposure Control Plan
RSD Pandemic Response Plan
Comprehensive Communicable Disease Management Plan
Introduction
Introduction
The health and safety of all students and staff is a priority of Reynolds School District (RSD). Vigilance and mitigation measures regarding communicable diseases promote health and wellness in the school setting. Providing a safe, comfortable, and healthy environment facilitates the educational process, encourages social development, and allows children to develop healthy attitudes toward school (NRC, 2020).
Illness and injury are not uncommon in the school setting and thus policies, procedures, and guidance regarding infection control are of utmost importance. When children are injured or feel unwell at school, it can create a risk to others and impact the ability of a child to fully participate in their educational activities. The Center for Disease Control’s Whole School, Whole Community, Whole Child model addresses health in schools. This model is student centered and emphasizes the role of the community in supporting the school, the connections between health and academic achievement and the importance of evidence-based school policies and practices (CDC, 2023).
The purpose of this comprehensive guide is to provide infection control guidance, practice standards, and protocols for MESD and its component school districts.
This document combines the district’s Communicable Disease Prevention Plan, Exposure Control Plan, and Pandemic Response Plan to form a Comprehensive Communicable Disease Management Plan. The district Exposure Control Plan in this manual discusses Standard Precautions in detail as well as Transmission Based Precautions which include
contact, droplet, and airborne precautions. The Exposure Control Plan in this manual is published by MESD to provide information on the development of an appropriate Exposure Control Plan. The manual is not intended as a substitute for a district’s own careful review of OR-OSHA regulations, which should be the basis for plan development. Agencies/Districts contracting with School Health Services for Bloodborne Pathogens Training may copy and/or revise all forms within this manual to meet their individual needs. The District Pandemic Plan will address measures specific to novel virus response.
Communicable Disease Prevention Plan
Communicable Disease Prevention Plan
Communicable disease control and prevention is of significant importance in creating a safe and healthy environment for students and staff.
A communicable disease is an infectious illness that is transmissible by: 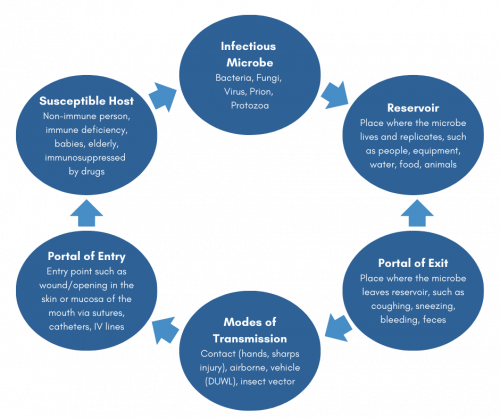
- Contact with bodily discharge or fluids of an infected individual
- Contact with contaminated surfaces or objects
- Inhalation of respiratory droplets expelled by an infected individual
- Ingestion of contaminated food or water
- Direct or indirect contact with disease vectors
Although the terms communicable disease, contagious disease, and contagious condition are often used interchangeably, it is important to note that not all communicable diseases that are spread by contact with disease vectors are considered to be "contagious" diseases since they cannot be spread from direct contact with another person (ACPHD, 2013). In the school setting there is a prevention-oriented approach for communicable disease management which is grounded in education, role modeling, and implementation of standard precautions and hygiene. However, population-based settings, such as the school setting, should establish practices for measures and interventions associated with exposures or potential exposures. This first section focuses on a population-based set of practices for communicable disease prevention, while the subsequent Exposure Control Plan discusses work-practice control measures for staff, per the OSHA Bloodborne Pathogen Standard (BBP, 29 CFR 1910.1030).
RSD Board Policies
Communicable Diseases JHCC
Communicable Diseases – Staff GBEB-AR
Communicable Diseases – Staff GBEB
Communicable Diseases – Students JHCC
Student Health Services and Requirements JHC
MESD Board Policies
The following board policies outline how the MESD navigates communicable diseases within their sites, per Oregon Legislation:
Communicable Diseases JHCC/EBBA/GBEB-AR
Communicable Diseases – Students and Staff JHCC/GBEB
School Health Services and Requirements JHC
Oregon Legislation
The following Oregon Administrative Rules (OARs) have been utilized to guide the information within this document and MESD board policies:
OAR 333-019-0010 Disease Related School, Child Care, and Worksite Restrictions: Imposition of Restrictions
OAR 581-022-2200 Health Services
Oregon Health Authority & Oregon Department of Education
Oregon Department of Education Communicable Disease Guidelines for Schools
Communicable Disease Prevention
Communicable Disease Prevention
There are a multitude of methods that can be applied to control communicable diseases at a variety of levels. Some of the most common include vector control, hygiene, sanitation, and immunization. Fully endorsing the control and prevention of communicable diseases requires an understanding of disease transmission.
How these communicable diseases are spread depends on the specific infectious agent. Common ways in which communicable diseases spread include:
-
Physical contact with an infected person, such as through:
- Touch (staphylococcus)
- Sexual intercourse (gonorrhea, HIV)
- Fecal/oral transmission (hepatitis A, C. difficile)
- Respiratory droplets (influenza, varicella-zoster)
-
Contact with a contaminated:
- Surface or object (norovirus)
- Food (salmonella, E. coli)
- Blood (HIV, hepatitis B, hepatitis C)
- Water (cholera, listeria)
- Bites from insects or animals capable of transmitting the disease (mosquito: malaria and yellow fever; flea: plague)
- Inhalation of small respiratory droplets that are dispersed through or suspended in the air (measles, tuberculosis)
In the school setting the most frequent risks are associated with direct contact with ill individuals, contaminated surfaces, or inhalation of infectious droplets. Primary methods of illness prevention include hand hygiene, sanitation, respiratory etiquette, isolation and exclusion of symptomatic individuals, as well as standard and transmission-based precautions.
This section of the plan will provide a brief overview of, and procedures on addressing the following communicable disease issues in the school setting:
- Common Childhood Infectious Disease
- Vaccines
- Hand Hygiene
- Respiratory/Cough Etiquette
- Environmental Surface Cleaning
Common Childhood Infectious Diseases
There are a variety of common childhood infectious diseases that are regularly encountered in the school setting. Some childhood illnesses such as the common cold (i.e.: adenoviruses, coronaviruses, rhinoviruses), bronchitis, sinusitis, and tonsillitis occur throughout the year. While other illnesses such as gastroenteritis (i.e.: norovirus), croup (i.e.: parainfluenza), and influenza (A & B) most often occur seasonally. Examples of other common childhood infections include: strep throat, hand foot and mouth disease, fifth disease, and staph skin infections. There are more severe infectious diseases, such as bacterial meningitis, that also occur sporadically throughout the school year (BCDC, 2021).
Vaccines
In the school setting, vaccines are an important step toward preventing and reducing the severity of communicable diseases. Certain vaccines are required for attending school in Oregon. However, it is important to note that some individuals may not be vaccinated due to medical/non-medical exemptions. Each school has a record of which students are and are not vaccinated with routine childhood immunizations as a primary control measure for outbreaks of vaccine preventable diseases. More information specific to
immunizations can be found on RSD's Immunizations webpage.
Hygiene
Prevention-oriented measures are grounded in disease transmission education, and the practical application of general sanitation and personal hygiene. Hygiene a nd sanitation are some of the most important methods of disease prevention. Handwashing is the single most important method of keeping germs at bay, specifically in the school setting. Appropriate handwashing practices should be taught to all students, modeled by staff, and practiced by all.
nd sanitation are some of the most important methods of disease prevention. Handwashing is the single most important method of keeping germs at bay, specifically in the school setting. Appropriate handwashing practices should be taught to all students, modeled by staff, and practiced by all.
Age appropriate hand hygiene curriculum can be found from a variety of resources and should be provided annually in the fall and as needed during peak illness season or specific increases of disease in the school setting.
Hand sanitizer, while not effective against a large number of pathogens, should be made available for times that handwashing is not immediately accessible. Hand sanitizer that contains at least 60% alcohol, should be easily accessible throughout the building, specifically in high contact areas such as entrances/exits, water fountains, cafeterias, gyms, and classrooms. Supervised stocks of hand sanitizer should be available in each classroom.
|
Students and staff should wash hands:
When immunocompromised students and staff are present, increase in hand hygiene frequency is a necessary illness-prevention intervention. |
Respiratory Hygiene / Cough Etiquette
Respiratory hygiene and cough etiquette are terms used to describe infection prevention measures to decrease the transmission of respiratory illness (e.g., COVID-19, influenza,  and cold viruses). A respiratory infection can be spread when a person who is infected coughs or sneezes. The droplets released from an ill person’s cough or sneeze can travel for
and cold viruses). A respiratory infection can be spread when a person who is infected coughs or sneezes. The droplets released from an ill person’s cough or sneeze can travel for
several feet, reaching the eyes, nose, or mouth of others, causing illness. Pathogens can spread easily from person to person through direct contact via touching contaminated objects or shaking hands with an ill individual, and then touching one’s eyes, nose, or mouth. Droplets can persist for some time on a variety of objects and high-contact areas, such
as doorknobs or desks. Some individuals cough without having a respiratory infection (e.g., persons with chronic obstructive lung disease), while others can carry and spread diseases without ever showing any symptoms of illness. As a result, we do not always know who is infectious and who is not. Therefore, respiratory hygiene and cough etiquette
are crucial/significant measures to protecting yourself from illness and preventing others from becoming ill. Like hand hygiene, respiratory hygiene is part of the standard precautions that should be taught, practiced, and modeled to prevent the spread of disease.
(Image: CDC)
Environmental Surface Cleaning
Clean schools contribute to healthy environments and reduce the risk of communicable disease transmission. Some of the important concepts associated with reduction in illness include:
- Scheduling and documenting the routine cleaning of classrooms, common areas, and shared objects and surfaces
- Ensuring adequate stock of appropriate sanitizers and disinfectants
- Ensuring garbage and sharps containers are emptied before they become full
- Ensuring that any classrooms with pets have a cleaning plan in place to minimize odors or contamination.
- Increasing ventilation and air filtration in classrooms to mitigate airborne and droplet transmission.
While environmental cleaning is largely governed by facilities management and custodial services, there are certain classroom measures that can be practiced to improve cleanliness and reduce the risk of illness-transmission during peak illness times, such as increasing access to sanitizing wipes, tissue, and hand sanitizer. (See the Exposure Control Plan for more detail on disinfection)
Communicable Disease Exclusion
Communicable Disease Exclusion
In the school environment, communicable diseases are easily transmitted from one individual to another by various routes, and can even be transmitted while an individual is not showing symptoms of illness. While some conditions are restrictable based on diagnosis, more often early identification of signs and symptoms of communicable disease is of paramount importance to increase the health of the school population and decrease school absenteeism. Effective control measures include: education, avoidance of risk factors, sanitation, air filtration/ventilation, vaccination, early recognition of symptoms, health assessment, prompt diagnosis, and adequate isolation and treatment (ODE, 2022).
Oregon public health law (Oregon Administrative Rule 333-019-0010) mandates that persons who work in or attend school who are diagnosed with certain diseases or conditions be excluded from school until no longer contagious. Since diagnosis often presumes assessment by a licensed health care provider and specific testing, schools must often make decisions regarding exclusion based on non-diagnostic but readily identifiable symptoms. As a matter of routine practice, individuals with any excludable symptoms of illness should be excluded from school per OAR 333-019-0010, LPHA guidelines, and the Oregon Department of Education Communicable Disease Guidance Document.
Restrictable Diseases
Restrictable diseases are specific infectious disease diagnoses that require students or staff to remain at home for a specified amount of time to limit transmission. Restriction is typically associated with the communicability or severity of a disease. Some restrictable diseases are also reportable to the LPHA [See: Table 1], in such an event the MESD Communicable Disease Team should always be contacted. The LPHA also notifies the MESD Communicable Disease Team of confirmed cases of reportable illness in a student or staff member. There are occasions when a parent/guardian will notify the school of a communicable disease first. In these cases the school nurse (RN) and building administrator should be notified and they will consult with the MESD Nurse Consultant. Students with diagnoses of diseases restrictable by the LPHA under OAR 333-019-0010 should return to school as directed by the LPHA and/or MESD Nurse Consultant.
| Diagnosis | LPHA Reportable? |
| Diphtheria | Yes |
| Hepatitis A | Yes |
| Hepatitis E | Yes |
| hMPXV (mpox) | Yes |
| Measles | Yes |
| Mumps | Yes |
| Pertussis (whooping cough) | Yes |
| Rubella | Yes |
| Salmonella enterica serotype Typhi infection | Yes |
| Scabies | No |
| Shiga-toxigenic Escherichia coli (STEC) infection | Yes |
| Shingellosis | Yes |
| Varicella zoster (chickenpox) | No |
| Infectious tuberculosis | Yes |
Reporting Restrictable Diseases
If a report is made to the school office, administration, or other school staff regarding any communicable disease diagnosis in students or staff:
- This should be regarded as an urgent referral to the MESD Nurse Consultant if the disease is a reportable condition and immediately be referred to the school nurse and building administrator (who should then consult with the MESD Nurse Consultant).
- Confidentiality rules should be followed. Information is not to be shared with students, staff, or parent(s)/guardian(s) of the report unless directed by the MESD Nurse Consultant.
- The MESD Nurse Consultant will confirm the diagnosis with the LPHA, and identify the need for communication, surveillance, or control measures.
- Depending on the diagnosis and the identified interaction with a reported case, the MESD Nurse Consultant may ask that the school nurse, or building administrator, directly notify any individuals who are at high-risk of severe disease, immunocompromised, or pregnant, so that they can reach out to their healthcare provider with any questions or concerns regarding a potential exposure.
The interventions and communication are driven by multiple factors including the diagnosis, student health status, risk of exposure, number of individuals infected, and risk to cohorts or specific students and staff.
Isolation Spaces
Oregon law (OAR 581-022-2220) requires the school district to maintain a prevention oriented health services program, which includes health care and space that is appropriately supervised and adequately equipped for first aid, and isolates the sick or injured child from the student body. An appropriate isolation space as described in the Communicable Disease Plan and consistent with state legislation should be accessible in each building. The intent is to mitigate the risk of transmission from an ill individual to well individuals. The isolation space should be logistically accessible in proximity to the health room, but not in such close proximity that infection risk is a concern.
CDC guidelines should be visited with the following five requirements in mind:
- Isolation space must be separate from routine health room
- Isolation space must have appropriate ventilation
- Students must be supervised while in isolation space
- Staff must have appropriate PPE while in the isolation space
- Appropriate physical distancing and confidentiality must be maintained in the isolation space
| Isolation Room | Consideration |
| Physical distance | It is strongly recommended that ill students are physically distanced while in the isolation space to the greatest extent possible. |
| Cleaning and sanitizing | After dismissal of ill student, close off areas used by a sick person and do not use these areas again until after cleaning and disinfecting. Ensure safe and correct use and storage of cleaning and disinfection products, including storing products securely away from children. |
| Ventilation | Designated isolation space should have adequate ventilation, i.e. exterior windows, ventilation fans and/or HEPA filters. Ensure fans do not re-circulate into air supply; vent to exterior or into non-communicating space (e.g. wall voids, attic). |
| Hand hygiene | Staff providing care should wash hands frequently and thoroughly before and after providing care, including after removal of gloves. Ensure isolation space has ready access to soap and water. Sink at the entryway is preferred. If soap and water is not accessible, use hand sanitizer with ≥60% alcohol content and wash hands with soap and water as soon as possible. |
| PPE |
Staff tending to symptomatic individuals should wear, at a minimum, a face mask. Gloves should be worn if there is risk of exposure to blood and body fluids. A face shield should be worn if there is a risk of body fluids splashing towards the face. A face shield should be worn if there is a risk of body fluids splashing towards face. Any PPE used during care of a symptomatic individual should be properly removed and disposed of prior to exiting the isolation room, and hands washed after removing PPE. |
| Student safety and well-being | Adjust protocols to age and developmental abilities. Ensure line of sight; keep the ill student visible. To reduce fear, anxiety, or shame related to isolation, provide a clear explanation of procedures, including use of PPE and handwashing. |
| When students are identified with restrictable diseases or excludable symptoms, they should be separated from the well-population, in an appropriate space until they can be dismissed to home. This isolation space should be separated from the healthcare area used to assess and treat injured and non-symptomatic children or to provide medication management and care of chronic healthcare conditions. |
Outbreaks of Illness, and Symptom Clusters
Outbreaks of Illness, and Symptom Clusters
Outbreaks are most often defined as compatible diagnoses or syndromes in individuals from 2 or more households that are epidemiologically-linked and in the same communicability time period. Because of the nature of the ongoing congregate setting of school, this definition is insufficient for the purposes of seasonal illness; rather an increase in morbidity or severity should be indicators to report to the school nurse and MESD Communicable Disease Team for consideration of outbreak reports or control measure implementation. The attention to outbreaks, interventions, and resources are highly dependent on the prevalence, severity, and communicability of the disease. Outbreak investigations will be facilitated through the MESD Communicable Disease Team, in collaboration with the school nurse, health assistant, building administrator, and the LPHA with the use of the Oregon Health Authority Outbreak Toolkits for Schools.
Respiratory Illness
Respiratory illness or disease refers to the pathological conditions affecting the organs and tissues that make gas exchange possible, including conditions of the upper respiratory tract, trachea, bronchi, bronchioles, alveoli, pleura and pleural cavity, and the nerves and muscles of breathing. Respiratory diseases range from mild and self-limiting, such as the common cold, to life-threatening, like bacterial pneumonia
|
Individuals with respiratory illnesses are often present in the school setting. The following indicators should be reported to the school nurse, who will consult with the MESD Communicable Disease Team:
*In the event of respiratory illnesses related to novel viruses, the Pandemic Plan will be deferred to. |
Vaccine Preventable Disease
A vaccine-preventable disease (VPD) is an infectious disease for which an effective preventive vaccine exists. Current VPDs routinely immunized for in the United States include:
|
|
|
Most VPD’s are also reportable diseases*, meaning they are under constant surveillance and the LPHA should be notified of any case. When a positive case of a vaccine preventable disease is identified in the school setting, or when the circulation of a vaccine preventable disease is increasing in incidence in a building or in the community, the MESD Nurse Consultant will work with the LPHA to determine the necessity for exclusion of unvaccinated students or staff, as needed, and notification of exposure to members of the school community. Staff may be asked to run immunization reports to identify unvaccinated students in the building.
Some communicable diseases are uncommon locally, and are not routinely immunized for in the US, so a diagnosed case would be of interest. This may include:
|
|
Uncommon diseases may also pose a risk to a susceptible individual or population if circumstances permit exposure, and should therefore also be reported to the LPHA.
|
Reports of VPDs should be referred to the MESD Nurse Consultant, whether coming from a parent, provider, community member, or the local public health authority (LPHA). Indicators for possible nurse consultant report to the health department of school-identified VPDs include:
|
Gastroenteritis
An outbreak of gastroenteritis is defined as three (3) or more cases of vomiting/diarrhea in a cohort (regardless of size). For example, three (3) children in a 25-person classroom with vomiting or diarrhea within one week could potentially indicate an outbreak. Because the nature of viral gastroenteritis (norovirus) is common, seasonal, and highly infectious, it is unlikely to result in an outbreak investigation unless the number infected and/or duration is unusual. However, preventive measures to reduce spread would need to be immediately enhanced and enforced. Because symptoms of bacterial gastroenteritis may start with a similar presentation, it is important to evaluate the severity for the duration of illness.
|
Gastrointestinal indicators to report to the school nurse include:
|
Other Circumstances
Less commonly, outbreaks of skin infections or other novel diseases occur, or unusual infectious disease circumstances arise.
|
To ensure the appropriate disease intervention, surveillance, and data collection occur, these unusual situations should be referred to the MESD Nurse Consultant and will be handled on a case by case basis. Examples of these circumstances may include:
|
In regard to determined outbreaks or novel diagnoses, the MESD Communicable Disease Team may decide that additional control measures or data collection are necessary, and will consult with the building administrator, the school nurse, and the LPHA as needed.
The MESD Nurse Consultant should always be consulted regarding any written communication that may be developed to notify parents, students, or staff about illness, disease outbreaks, and risks to students, families, and staff, and/or control measures specific to an outbreak or exposure. Any presentation of illness or combination of illnesses as described above should be reported to the MESD Nurse Consultant and the building administrator.
Disease-Specific Guidelines
Disease-Specific Guidelines
Follow recommended actions when a health care provider has diagnosed a communicable disease, or a person exhibits related symptoms.
NOTE: This document is not a diagnostic tool. Related symptoms may inform exclusion decisions, but school staff do not diagnose.
Restrictable diseases require school exclusion. If the student or staff has any of the following diseases, then clearance by the local public health authority is required before the individual returns to school: chickenpox, diphtheria, Hepatitis A, Hepatitis E, measles, mumps, pertussis (whooping cough), rubella, Salmonella enterica serotype Typhi infection, scabies, Shiga-toxigenic E. coli (STEC) infection (O157 and others), shigellosis, and infectious tuberculosis.
Oregon public health laws regulate which diseases are “restrictable” and/or “reportable.”
|
DISEASE/SYMPTOMS |
SCHOOL EXCLUSION/ SCHOOL RESTRICTION and REPORTING TO LOCAL PUBLIC HEALTH AUTHORITY |
TRANSMISSION/ COMMUNICABILITY |
RECOMMENDED SCHOOL CONTROL MEASURES |
|
ATHLETE’S FOOT
|
Exclude: NO. Restriction: NO. |
Spread by:
Communicable:
|
|
|
CHICKENPOX (Varicella)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines and see below. Restriction: YES. Exclude until chickenpox lesions have crusted or dried with no further drainage (minimum of 5 days after rash appears). |
Spread by:
Communicable:
|
|
|
COMMON COLD (Upper/Lower Respiratory Infection)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: NO. |
Spread by:
Communicable:
|
|
|
COVID-19
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: NO |
Spread by:
Communicable:
|
|
|
DIARRHEAL DISEASES
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: Exclude students with acute diarrhea. Diarrhea with diagnosis of E. coli, Salmonella, or Shigella, requires school exclusion until cleared for return per local public health authority. |
Spread by:
Communicable:
|
|
|
FIFTH DISEASE
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider permission or when no rash or signs of illness are present. |
Spread by:
Communicable:
|
|
|
HAND, FOOT & MOUTH DISEASE Sudden onset fever, sore throat, and lesions affecting mouth, hands, feet, and genitals. |
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider permission or when blisters have healed. |
Spread by:
Communicable:
|
|
|
HEAD LICE
|
Exclude: Refer to CDC guidance on head lice. Restriction: NO. |
Spread by:
Communicable:
|
|
|
HEPATITIS A & E
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restricted: YES. May attend only with local public health authority permission. |
Spread by:
Communicable:
|
|
|
HEPATITIS B & C
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: NO. Restriction may apply to “hepatitis B infection in a child, who,in the opinion of the local health officer, poses an unusually high risk to other children (for example, exhibits uncontrollable biting or spitting)” [OAR 333-019-0010] |
Spread by:
Communicable:
|
|
|
HIV Disease (Human Immunodeficiency Virus Disease)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: NO. |
Spread by:
Communicable:
|
|
|
IMPETIGO
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider permission, or when lesions are dry and crusted with no drainage. |
Spread by:
Communicable:
|
|
|
INFLUENZA (flu)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: NO. |
Spread by:
Communicable:
|
|
|
MEASLES
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: YES. May attend with local public health authority permission. |
Spread by:
Communicable:
|
|
|
MENINGOCOCCAL DISEASE
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend after treatment and clearance from provider. Patients are not contagious after treatment. |
Spread by:
Communicable:
|
|
|
MONONUCLEOSIS
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restrictions: NO –Withdrawal from PE/Athletic activities may be recommended by licensed health care provider permission. |
Spread by:
Communicable:
|
|
|
MUMPS
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: YES. May attend with local public health authority permission. |
Spread by:
Communicable:
|
Immunization Requirements for School and Child Care | Getting Immunized
|
|
PERTUSSIS (Whooping Cough)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: YES. May attend only with local public health authority permission. |
Spread by:
Communicable:
|
Immunization Requirements for School and Child Care | Getting Immunized
|
|
PINK EYE (Conjunctivitis)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider/school nurse permission or symptoms are gone. |
Spread by:
Communicable:
|
|
|
PINWORMS
|
Exclude: NO Restriction: Restriction may be necessary in situations where students are unable to control bowel function, otherwise No. |
Spread by:
Communicable:
|
|
|
RINGWORM – SCALP
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider or school nurse permission or when symptoms are gone. |
Spread by:
Communicable:
|
|
|
RINGWORM – SKIN
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider or school nurse permission or when symptoms are gone. |
Spread by:
Communicable:
|
|
|
SCABIES
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: YES. May attend with licensed health care provider/school nurse permission. |
Spread by:
Communicable:
|
|
|
SHINGLES (Herpes Zoster)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider permission and if lesions can be covered with dressing or when lesions are scabbed/dried. |
Spread by:
Communicable:
|
|
|
STAPH SKIN INFECTIONS
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider permission or when lesions are dry/crusted or gone. |
Spread by:
Communicable:
|
|
|
STREP THROAT & SCARLET FEVER
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: May attend with licensed health care provider/school nurse permission. |
Spread by:
Communicable:
|
|
|
TUBERCULOSIS (infectious/active)
|
Exclude: Refer to Symptom-Based Exclusion Guidelines. Restriction: YES. May attend only with local public health authority permission. Note: tuberculosis can be chronic/latent; is only restrictable in the infectious/active stage. |
Spread by:
Communicable:
|
|
Section References
Centersfor Disease Control and Prevention. COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed May 2023.
Centers for Disease Control and Prevention. Definitions of Symptoms for Reportable Illnesses.
https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html. Published June 30, 2017.
Centersfor Disease Control and Prevention. Type of Duration of Precautions Recommended for Selected Infections and Conditions.
https://www.cdc.gov/infectioncontrol/guidelines/isolation/appendix/type-duration-precautions.html. Published July 22, 2018
Animals in School
Animals in School
Animals in schools can have a positive effect in the school environment, but may also cause infectious disease issues or other issues for staff and students. District policy and/or procedures should be followed regarding animals in school buildings. The following considerations should be made in regard to controlling the spread of infectious diseases from animals:
-
Wild mammals, alive or recently dead, should not be allowed in
 the school setting. Bats and skunks have a
the school setting. Bats and skunks have a
significant risk of being rabid. Other wild animals may be more prone to causing injury through bites and scratches. - Dogs, cats, and ferrets allowed in school buildings should have a current rabies vaccine.
- Any animal bites on school property should be reported to the LPHA for follow up. Standard first aid should be provided and the individual should be referred to their health care provider.
- Animals who are ill should not be allowed into the school setting.
- Class pets should be removed if they become ill.
- Handwashing must occur before and after handling of animals to prevent disease transmission.
- Animals should not be present or handled in areas where food and drink are consumed or prepared.
- Children should not kiss high risk animals such as chicks, ducks, turtles, and other reptiles.
- Children should always be monitored during animal interactions.
- Consider the medical needs of students who are immunosuppressed or who have allergies, as they may become severely ill when exposed to certain pathogens or allergens.
- In the event that a student in a classroom is diagnosed with a disease known to be carried by animals (i.e., campylobacteriosis or salmonellosis), any classroom animals should be removed from the classroom setting until the risk is determined to be resolved.
Food Safety
Food Safety
Food safety training and enforcement for nutrition services staff is supervised by nutrition services. For the overall wellness of our school-based population, all food preparation and consumption within the classroom should follow general food safety standards and disease prevention principles. 
For elementary school classrooms
- Hand hygiene is enforced prior to eating
- General principles of food safety can be taught that are age appropriate
- Food sharing should not be allowed
- For classroom and school sponsored events, only commercially prepared products are permitted. Do not allow homemade food from non-licensed kitchens to be served
For middle school or high school culinary classrooms:
- Hand hygiene should always be enforced
- Age appropriate food safety principles are taught
-
Appropriate food handling processes must be taught, role modeled, and enforced. This includes overview of:
- Hand hygiene and appropriate use of gloves
- Clean surfaces and appropriate use of sanitizers
- Separating raw and ready to eat foods / avoidance of cross contamination
- Cooking food to appropriate temperatures
- Appropriate storage and refrigeration
- Measures to prevent allergic reactions
- Abstaining from food preparation when specific symptoms or specific illnesses have been identified
Exposure Control Plan
Exposure Control Plan
This plan provides the employees of RSD with guidelines for handling any exposure to blood or other potentially infectious materials (OPIM). These established procedures are in accordance with local and state requirements, as well as federal occupational safety and health requirements (OSHA BBP Standard 1910.1030).
The principle of Standard Precautions holds that all body fluids or other potentially infectious materials should be considered potentially infectious at all times, since many disease-causing pathogens may be carried in the body fluids of persons who show no symptoms of illness. Standard Precautions shall be observed in all RSD sites in order to prevent contact with all body fluids and other potentially infectious materials including: blood, semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids. Transmission-Based Precautions should additionally be endorsed in circumstances where specific risk is anticipated based on health status.
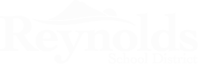
Disease transmission is facilitated by three conditions: high infectivity of a body fluid from an infectious person (carrier), a portal of exit from the carrier, and a portal of entry into a susceptible person. Any staff who may be expected to clean up body fluid spills, perform personal care for a student, perform initial first aid or injury response, or who are working with populations less able to control their bodily fluids in a congregate setting (such as a school), are reasonably anticipated to have “occupational exposure” to blood or other potentially infectious material. These staff should be provided the required training and personal protective equipment (PPE) so that they are aware of their risks and are able to best protect themselves.
RSD Board Policies
EBBAA - Infection Control and Bloodborne Pathogens
GBEB Communicable Diseases in Schools
GBEB-AR Communicable Diseases in Schools
OSHA
Bloodborne Pathogens 1910.1030
Personal Protective Equipment 1910 Subpart 1
Exposure Prevention
Exposure Prevention
Per OSHA regulations, in order to reduce risk and promote prevention of infections related to blood or body fluids, the district will provide and promote specific trainings or practices to prepare staff, including:
-
Blood Borne Pathogens (BBP) Training
- An annual requirement for all at-risk staff.
- The first class must be taken with an instructor presenting the class, and the subsequent annual updates may be taken online through MESD’s website1 between the hours of 8:00 AM- 4:30 PM.
-
Hepatitis B vaccination
- Education and recommendations on Hepatitis B Vaccination are provided each year with BBP training.
- If staff opt out of receiving the Hepatitis B vaccin after completing the in-person BBP training, a waiver may be signed in lieu of immunization acknowledging their understanding of the risk and implications.
-
Standard Precautions
- Consistent use of Standard Precautions is expected any time the risk of exposure to body fluids is present.
- Routine training, refreshers, and understanding of appropriate first aid.
- Routine training or refreshers for staff who provide direct care to students or who work with students with specific disabilities, and/or health or behavior plans.
1 Please note that the Safe Schools/Vector BBP Module, while a good general course for all school staff to take, is not an OSHA-approved training that meets the requirements for the training of at-risk staff.
Employee Exposure Determination
Employee Exposure Determination
Any employee with a risk of occupational exposure to blood and other potentially infectious body fluids is protected by the OSHA-required EXPOSURE CONTROL PLAN. Exposure determination for common job classifications in schools are noted below. Exposure determination of school employees is the responsibility of the school or district administrator. School districts must review job tasks and make individual determinations regarding exposure risks based on OR-OSHA criteria. Each school environment will need an individual assessment of risks to various employees. School administrators may need assistance with determination of risk for certain employees due to their specific job tasks and are encouraged to seek consultation with the MESD Nurse Consultant, the local public health authority, the district risk management department, or legal counsel regarding this risk of exposure.
CLASS A EXPOSURES: Job classifications in which employees are assumed to have occupational exposure due to direct physical care in which blood or other potentially infectious material could be present (such as direct care for injuries, illnesses, medical/dental procedures, injections, etc.). This may include:
- School Health Services staff in health-rooms or isolation spaces
- Secretaries or other office assistants in schools without available health services staff
- Custodial staff or any other staff expected to clean up body fluid spills
- Athletic Trainers/Coaches/P.E. Teachers dealing with acute injuries
- Unlicensed Assistive Personnel (UAP) who provide tasks taught or delegated by the school nurse
- Staff working with Special Education (SpEd) populations or other populations who are not able to adequately contain their body fluids, or who expose others through behaviors such as biting, spitting, fecal smearing, and scratching .
- Staff who have a job description which requires them to provide first aid to students/staff
CLASS B EXPOSURES: Job classifications in which employees may be expected to have some occupational risk. This may include:
- General Educational Teachers/Educational Assistants & Substitutes
- School Psychologist
- Physical/Occupational Therapists
- Speech Language Pathologists
- Students and Instructors in Health Occupation Programs
- Bus Drivers
Please note: It is the responsibility of the individual school district administrator to determine which school employee job descriptions place employees at risk for body fluid exposure.
Universal & Standard Precautions
Universal & Standard Precautions
The premise of Universal Precautions is to treat all body fluids as potentially infectious. Standard Precautions align with this and provide a set of standards for hygiene and barrier protection (or PPE) during any and all encounters with body fluids.
Standard Precautions are regarded as the minimum infection prevention practices that apply to all direct care or exposure to body fluids, regardless of suspected or confirmed infection status of the individual, in any setting where there is an expected risk of body fluid exposure. In the school setting, body fluid exposures most frequently occur with physical injury or acute illness. Exposures may also occur relative to a chronic health condition, medical procedure, developmental delay, behavioral issue, or disability. Students and staff/volunteers should be encouraged to care for their own bleeding injuries. If assistance is necessary, the use of disposable gloves and other barriers, followed by hand washing, is required for the designated caregiver when body fluids are present. There may be occasions when unanticipated contact with body fluids will occur, and in such cases, staff should follow the MESD Body Fluid Exposure Protocol (to be discussed below).
Standard Precautions endorse the appropriate use of PPE and other practices such as hand hygiene and respiratory etiquette, as well as work practice controls such as sharps safety (i.e., handling needles, lancets, broken glass, etc.) and environmental disinfection.
Hand Hygiene
Hand hygiene is the most important measure to prevent the spread of infections. In the school setting hand hygiene is an important infection prevention method as a matter of habit with restroom use and food preparation and consumption. Encourage school staff to teach, model and provide structured time for students to practice appropriate hand washing. In the context of BBP and exposure control, hand hygiene should be enforced each time a staff member has an interaction with a student for standard first aid, medication administration, or direct care. Hands should be washed prior to donning gloves, and after care is completed and gloves are removed.
Personal Protective Equipment (PPE)
PPE refers to wearable equipment that is designed to protect staff from exposure to or contact with infectious agents. PPE that is appropriate for various types of interactions and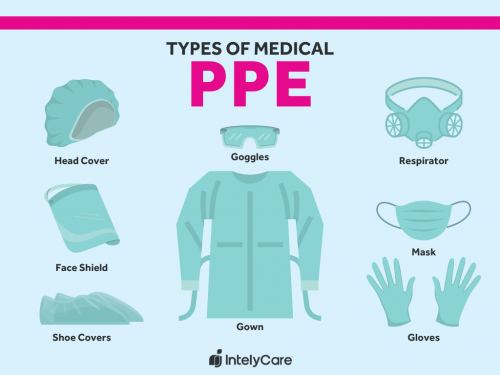 effectively covers personal clothing, skin and mucous membranes (eyes, nose, mouth) likely to be soiled with blood, body fluid, or other OPIM should be available to school staff, in the appropriate sizes. These include gloves, face masks, protective eyewear, face shields, CPR masks, Kevlar sleeves or bite guards, and protective clothing (e.g., reusable or disposable gown). Contaminated PPE must be removed and disposed of before further contact with other surfaces or individuals occurs.
effectively covers personal clothing, skin and mucous membranes (eyes, nose, mouth) likely to be soiled with blood, body fluid, or other OPIM should be available to school staff, in the appropriate sizes. These include gloves, face masks, protective eyewear, face shields, CPR masks, Kevlar sleeves or bite guards, and protective clothing (e.g., reusable or disposable gown). Contaminated PPE must be removed and disposed of before further contact with other surfaces or individuals occurs.
Examples of appropriate use of PPE include:
- Use of gloves in all situations involving possible contact with blood or body fluids, mucous membranes, non-intact skin (e.g., exposed skin that is chapped, abraded, or with dermatitis), or OPIM. Gloves must be removed and replaced as soon as practical when they are contaminated, torn, punctured, or when their ability to function as a barrier is compromised. Always wash or sanitize hands before donning gloves and after glove removal.
- Use of gowns to protect skin and clothing during procedures or activities where contact with blood or body fluids is anticipated, such as diapering, toileting, feeding, suctioning, general cleansing, caring for a student who is actively vomiting or providing first aid.
-
Use of mouth, nose, and eye protection (such as a face shield, mask and eyewear) during activities that are likely to generate splashes or sprays of blood or other body fluids, such as:
- Feeding, providing care to, or assisting with a child with forceful vomiting or coughing.
- Suctioning a child with a tracheostomy with a history of forceful coughing or copious secretions.
- Assisting in the care of a student with a severe injury and spurting blood.
- Assisting a student with a head or facial wound.
- Assisting a student who displays erratic behavior that places the employee at risk (i.e. fighting, spitting).
- Use of Kevlar-sleeves or bite-guards when working with students with a history of biting or scratching behaviors.
- Use of mask or face shield when respiratory transmission is of concern (see pandemic plan).
| IF... | THEN... |
| It’s wet ( it’s infectious) | Wear gloves, wash hands before and after gloves |
| It could splash into your face | Wear a face shield |
| It’s spread through the air | Mask yourself and the student |
| It could splash on your clothes | Wear a gown |
| You are providing direct care or first aid | Wear gloves, wash hands before and after gloves |
| You are providing CPR | Use a barrier / CPR mask and gloves |
| There is a blood spill or body fluid spill | Request assistance from BBP-trained staff for appropriate disinfection |
Refer to the CDC’s Sequence For Putting on Personal Protective Equipment (PPE) for donning and doffing (Applying and Removing) PPE.
Respiratory Hygiene / Cough Etiquette
In the school setting, respiratory etiquette is an important measure to teach to staff and students as developmentally appropriate. Visual alerts, such as Cover Your Cough signage, can be used as a reminder for students and staff.
Appropriate respiratory etiquette includes practices on:
- Covering mouth and nose with a tissue when coughing or sneezing and then using the nearest waste receptacle to dispose of the tissue after use.
- Performing hand hygiene (e.g., hand washing with soap and water, alcohol-based hand sanitizer, or antiseptic hand wash) after having contact with respiratory secretions or contaminated objects/materials, such as a used tissue.
- Sneezing or coughing into the elbow joint (when a tissue and hand hygiene is not immediately accessible).
- Avoiding sneezing directly into the hands, where they may subsequently contaminate other items or surfaces.
-
Having symptomatic individuals placed in a designated isolation space where risks to others are minimized until dismissed to home. A mask should be offered and worn if tolerated. Spatial separation of the person with a respiratory infection from others is important since respiratory droplets travel through the air for an average of 3-6 feet.
To ensure these practices can be followed, each school should maintain the availability of materials for adhering to Respiratory Hygiene/Cough Etiquette in shared areas by:
- Providing tissues and no-touch trash receptacles for used-tissue disposal.
- Ensuring that supplies for hand washing (i.e., soap, disposable towels, sink) are consistently available.
- Providing conveniently located dispensers of at least 60% alcohol-based hand sanitizer where sinks are not available.
- Providing face masks for individuals with respiratory symptoms
Engineering and Work Practice Controls
Engineering and Work Practice Controls
Regulated (Biohazardous) Waste Containers
OR-OSHA defines regulated waste as “liquid or semi-liquid blood or other potentially infectious materials.” All school settings should be equipped with a regulated waste container to dispose of materials that are saturated with body fluids. There will be few items that are true regulated waste in a school setting, with the exception of contaminated sharps. Items with blood or other potentially infectious materials in a liquid or semi-liquid state, that if compressed would release liquid, must be disposed of in regulated waste containers that have a biohazard label.
Contaminated items that are exempt from regulated waste include: diapers soaked with urine or feces and feminine hygiene napkins (those fluids are absorbed and contained easily within the product). Determining what constitutes regulated waste (that must go into a biohazard-labeled container), versus contaminated waste (that can be disposed of in the regular trash), requires some independent decision and judgment. If waste soiled with blood or body fluids, as identified in the OR-OSHA definition of other potentially infectious materials, is saturated to the point of dripping, or would release fluids under compression, it needs to be identified, handled, and discarded as regulated waste. It is recommended that extra absorbent materials be utilized to clean up large body fluid spills, so that the waste is not liquid or dripping, and can therefore be disposed of in the normal trash as contaminated waste. School districts are encouraged to also review Oregon Statutes and Rules that govern the disposal of infectious waste.
Sharps Safety
Needle stick injuries (piercing the skin with a used needle) are a potential risk in any work environment where medications are delivered via syringe or compatible device, or where lancets are used. In the school setting this is most often associated with the care of students who have medical conditions that require injectable medications. It is preferred that students provide self-care for such high-risk tasks whenever feasible, however this is not always safe due to the capability of the student or for the administration of emergency medications. Staff must be appropriately trained by a nurse before using injection devices. Handling of sharp instruments is covered with designated staff in specific training relative to their job responsibilities.
Certain controls must be enforced in any situation where sharps are present to reduce the risk of needle sticks, including:
- Avoid using needles or lancets that must be taken apart or manipulated after use.
-
Do not recap, bend, or break one-time-use needles or other sharp devices. Two-hand manipulation of sharps is prohibited.
- For example, students needing glucose monitoring by use of a lancet device should be encouraged to remove the lancet from the device themselves. If the student is unable, the use of a tool, such as needle nose pliers or medical clamps/hemostat, is required to prevent hand contact with the contaminated sharp.
- Always dispose of used needles or lancets in a sharps container appropriately labeled with a biohazard sign immediately after use.
- Do not reuse needles and understand that most needles should only be used a single time.
- Participate in specific training related to injectable medications.
- ALWAYS use a needle-stick-prevention tool in cases where a multi-use injection pen needs to be recapped after use. NEVER hold a cap, vial, or other container with your fingers while bringing the needle or sharp object toward the cap, vial, or container.
- Do not walk with exposed sharps; instead take a portable sharps container to the location of the sharps for immediate disposal.
Contaminated sharps must be stored in closed puncture-resistant containers (sharps containers) with appropriate biohazard label and fill-line designation. It is best practice for sharps containers to be secured to a wall or countertop in the space that injections are given to students or where other sharps (lancets) are generally used. Additionally, schools may have a portable sharps container in the emergency kit and/or to use to retrieve a dirty sharp on school grounds. It is the responsibility of the district to ensure the provision of a sharps container for each school/location along with timely removal and replacement when containers become full.
Health Room, Isolation Space, and Classroom Safety
Eating, drinking, applying cosmetics or lip balm, and handling contact lenses are prohibited in potential exposure areas. Storage of food/beverages is prohibited in places where body fluids or other potentially infectious materials may come in contact with surfaces such as countertops, sinks, or refrigerators in health rooms. Health rooms, isolation spaces, and classrooms should strive to have furniture items and other surfaces that are made of materials that are easily disinfected, and move toward removing surfaces that cannot be easily cleaned between uses. Sinks used for first aid and health room purposes should not have dishes, cups, or utensils placed in them. If the only sink available in the health room area is the first aid sink, a separate clean water source should be used to medicate and hydrate students.
Cleaning and Disinfecting Environmental Surfaces
The cleanliness of the district facilities is the responsibility of facility and custodial services who have specific expertise in the appropriate formulations to use for specific circumstances. For this reason, any body fluid spills should be immediately referred to custodial services. Schools should determine and implement an appropriate written schedule and documentation log for cleaning and decontamination of high contact surfaces and areas that may be susceptible to contamination with blood or other potentially infectious material, such as the health room and isolation room.
In the event of a blood spill, blood spill kits should be accessible on all campuses. If custodial services are not immediately available, then another trained staff member who has gone through the in-person MESD BBP class should be called to clean the spill up immediately. Appropriate PPE should always be used with any body fluid clean up. Any articles used to clean body fluid spills must be handled with gloved hands and disposed of in an appropriate receptacle. If an absorbent agent is used, sweepings must be disposed of in a similar manner. Brooms and dustpans must be cleaned with a disinfectant. The CDC recommends using a freshly-mixed (no more than 24 hours old), diluted-bleach-solution (1 part bleach to 9 parts water) to disinfect areas with body fluid spills. Keep students away from areas being disinfected. If a bleach solution is not available, the school may use an EPA-approved tuberculocidal agent instead.
Steps for cleaning up a body fluid spill:
- Absorb the fluid spill.
- Wash the surface with a general cleaner.
- Ensure that all surfaces are visibly clean prior to using the disinfecting solution (or the solution may be rendered ineffective).
- Disinfect the area with a 1:10 bleach solution (or other EPA approved solution).
- Leave the disinfectant on the contaminated surface for 10 minutes for blood spills, or follow the manufacturer’s directions.
Using these basic principles, the management of spills should be flexible enough to cope with different types of spills, taking into account the following factors:
- The type of spill – sputum, vomit, feces, urine, blood or laboratory items
- The pathogens most likely to be involved in these different types of spills – stool may contain viruses, bacteria, or protozoan pathogens
- The size of the spill – spot (few drops), small (<10 cm), or large (>10cm) circumference
- The type of surface – carpet or impervious surface
- The location of the spill – (ie: contained area [such as a single office], common area or restroom)
- The likelihood of exposure – another person’s bare skin or mucous membranes were in contact with the spilled body fluid or with the contaminated surface
All disposal of biohazard waste will be in accordance with EPA guidelines. The directives for appropriate sanitizing and waste removal should come from the facilities department in coordination with a contracted, licensed refuse-disposal company.
Transmission-Based Precautions
Transmission-Based Precautions
When Standard Precautions alone cannot prevent transmission, they are supplemented with Transmission-Based Precautions. This second tier of infection prevention is used when there is a specific risk related to an ill student or staff in the school setting that can spread through contact, droplet, or airborne routes (e.g., skin contact, sneezing, coughing) and are always used in addition to Standard Precautions. While use of Transmission-Based Precautions are typically restricted to the health room/isolation space under specific conditions, there is still a risk of exposure in the school setting.
Contact Precautions
Contact Precautions are to be used when a student has a known or suspected illness that is easily transmitted by direct contact with the ill individual (or their body fluids) or by contact with contaminated items in their environment. Illnesses requiring contact precautions may include, but are not limited to, open and draining lesions, stool incontinence, uncontrolled secretions, vomiting, or a new generalized rash.
When a student presents with an illness that requires contact precautions the following steps should be taken:
- Ensure appropriate student placement: the student should be removed from the classroom setting and placed in the symptom space while awaiting parent/guardian arrival. Staff members should consult with their direct supervisor and be excused from their work duties.
- Use PPE appropriately: if the student requires care, gloves must be worn. A gown may be needed if the student’s body fluids are not controlled/contained.
- Limit student activity: the student’s activity should be limited to reduce additional opportunity for contamination of surfaces.
- Prioritize cleaning and disinfection: after the student has been dismissed to home, ensure the area the student was located during direct care and/or areas of body fluid spills are appropriately sanitized. If there is a risk of contamination in other settings such as the classroom, cafeteria, or playground, ensure areas and/or shared items are appropriately disinfected before use by others.
Droplet Precautions
Use Droplet Precautions when students or staff have a known or suspected infection transmitted by respiratory droplets. Droplets are generated by an individual who is coughing, sneezing, or talking. In the school setting this may be more common during influenza season and during the circulation of novel viruses.
- Source control: includes putting a mask on the ill student/staff member.
- Ensure appropriate placement: a student who becomes symptomatic when the risk of specific viruses is increased should be placed in the isolation room, individually (if possible), until arrival of the parent/guardian or until dismissed from school. Staff members should consult with their direct supervisor and be excused from their work duties.
- Use PPE: staff should wear a mask any time they are providing care to or screening a student / staff member who presents with respiratory symptoms and may consider wearing eye protection if the ill individual does not practice adequate respiratory etiquette.
- Limit activity of the ill student: the student or staff member’s activity should be should be limited and they should wear a mask to reduce additional opportunity for air and/or surface contamination.
Airborne Precautions
Use Airborne Precautions when students or staff have a known or suspected infection transmitted by the airborne route (e.g., measles, chickenpox). Airborne precautions will rarely be used in the school setting; however, it is important to use identified control measures as vaccine preventable respiratory diseases are on the rise related to increased vaccine hesitancy. It is important to note that the school district cannot compel anyone to immunize themselves or their student, but students and staff who are unvaccinated (or not up to date with their vaccines) can be excluded for the maximum incubation period of a vaccine-preventable disease, up to 21 days from their last exposure.
- Source control: includes putting a mask on the ill student / staff member.
- Ensure appropriate placement: the student should be placed in an isolation room, individually (if possible), with appropriate supervision.
- Use PPE: staff should wear a fit-tested NIOSH-approved N95 or higher level respirator when providing direct care or supervision of the student. If a fit-tested NIOSH-approved N95 is not available, then a medical-grade surgical mask should be worn.
- Limit activity: the student or staff member’s activity should be restricted to the isolation space, except to dismiss home.
- Notify the MESD Nurse Consultant: following contact with an individual identified as having a vaccine preventable disease, students or staff susceptible to any diagnosed infection, such as measles, pertussis, or varicella, should be advised to immediately seek immunization against infection and/or speak with their healthcare provider.
Body Fluid Exposure Incidents
Body Fluid Exposure Incidents
A body fluid exposure incident is an event where the potential exposure to infectious disease has occurred. This can occur through a variety of ways, but in the school setting this primarily occurs through contact with body fluids via mucous membranes or open, unprotected skin; through a human or animal bite; or through a needle stick injury.
When an exposure has occurred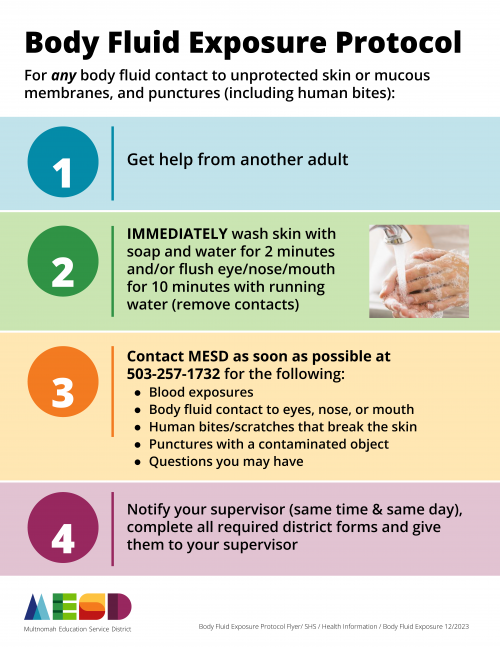
- Staff: should immediately clean the affected area and follow the MESD Body Fluid Exposure Protocol (below).
- Students: should receive basic first aid including cleaning the wound and/or flushing all affected mucous membranes. The building administrator should then call the parent/guardian and recommend they call the student’s healthcare provider with any concerns or questions. This should be followed up with a school district incident report completed by the staff member who witnessed or reported the exposure event.
Needle-Stick Injuries
If a staff member's skin is pierced or punctured with an object that may be contaminated with the body fluid of others, follow the MESD Body Fluid Exposure Protocol. Staff may be referred immediately to an occupational health clinic for further assessment and possible treatment, and may be required to report back to the provider for subsequent blood tests. Students should receive basic first aid including cleaning the wound/puncture site and then be referred to their healthcare provider.
Mucous Membranes
When there is any potential body fluid exposure toward the face, all exposed mucous membranes, including the nose, mouth, and eyes should all be immediately flushed with running water for at least ten minutes. Staff should follow the MESD’s Body Fluid Exposure Protocol.
Bites
While bloodborne pathogen transmission is less common via bites, there are concerns for tissue injury and/or of exposure to other infectious diseases. Staff should provide all necessary basic first aid and follow MESD’s Exposure Protocol. In the event of a bite injury, staff may be encouraged to seek urgent medical care depending on the severity of the bite. Dog bites should be reported to the Multnomah County Animal Control at (503) 988-7387 to assess for rabies.
The MESD Nurse will perform an evaluation of all occupational exposures as required by OSHA law and refer employees for immediate follow-up at an occupational health clinic as necessary. This follow-up appointment, and any resulting care, treatment, or future appointments resulting from an occupational exposure are to be paid for by the employing district. It is assumed that all employees will follow their training and protocol on body fluid exposures, and notify their district supervisor of all body fluid exposure incidents and whether or not they were referred by the MESD Nurse for follow-up care.
Pandemic Plan
Pandemic Plan
A pandemic occurs when an infectious disease has spread globally. Viruses, such as coronaviruses and influenza, are routinely surveyed due to the propensity for mutations, human to animal transmission, and potential for pandemic events. The purpose of this document is to provide guidance for Non-Pharmaceutical Interventions (NPIs) and their use during a novel viral respiratory pandemic. NPIs are actions, apart from getting vaccinated and taking medications, that people and communities can take to help slow the spread of respiratory illnesses such as pandemic flu or novel coronaviruses. NPIs, specifically in regard to pandemic planning, are control measures that are incrementally implemented based on the level of threat to a community. This document should be used as a contingency plan that is modified with a response planning team based on the current level and type of pandemic threat.
SEASONAL RESPIRATORY ILLNESS AND SEASONAL INFLUENZA
Seasonal Respiratory Illness
There are several viruses that routinely circulate in the community that cause upper respiratory illnesses. These viruses include rhinoviruses, coronaviruses, adenoviruses, enteroviruses, respiratory syncytial virus, human metapneumovirus, and parainfluenza. The “common cold” is caused by rhinoviruses, adenoviruses, and coronaviruses. The symptoms of these seasonal illnesses may vary in severity, but include cough, low-grade fever, chills, fatigue, runny notes and headache (CDC, 2024) .
Seasonal Influenza
Influenza (flu) is a contagious respiratory illness caused by influenza viruses. There are two main types of influenza (flu) virus: Types A and B. The influenza A and B viruses that routinely spread in people (human influenza viruses) are responsible for seasonal flu epidemics each year. Influenza can cause mild to severe illness. Serious outcomes of flu infection can result in hospitalization or death. Some people, such as older people, very young children, and people with underlying health conditions or weak immune systems, are at high risk of severe flu complications. Routine symptoms associated with flu include fever, cough, sore throat, runny nose, muscle aches, headaches, fatigue, and vomiting (CDC, 2022).
Novel, Variant, and Pandemic Viruses
Novel viruses refer to those not previously identified. A novel virus may be a new strain or a strain that has not previously infected human hosts. When a virus that has historically infected animals begins to infect humans it is referred to as a zoonotic virus. Pandemic refers to an infectious disease that has spread over a wide geographical area or worldwide. The most common viruses associated with novel and pandemic outbreaks are influenza A and human variants of coronaviruses. A flu pandemic occurs when a new variant that is different from seasonal viruses emerges and spreads quickly between people, causing illness worldwide. Most people will lack immunity to these viruses. Pandemic flu can be severe, causing more deaths than seasonal flu. Because it is a new virus, a vaccine may not be available right away. A pandemic could, therefore, overwhelm normal operations in educational settings (CDC, 2023).
Control Measures
Control Measures
While prophylactic vaccines and medications are appropriate interventions in some viral respiratory conditions, such as seasonal influenza and COVID-19, these are not always accessible for novel strains. NPIs are essential actions that can aid in the reduction of disease transmission. It is important to note that disease that is widely spread in the community has many options for transmission beyond the school setting, and the school district can only account for NPIs in the school setting and at school-sponsored events.
Everyday Preventive Measures
Control measures to limit the spread of communicable diseases should be an active part of the school comprehensive and preventive health services plan . Routine control measures include:
- Hand hygiene (washing your hands for 20 seconds with soap and water with appropriate friction).
- Respiratory etiquette (cover your coughs and sneezes with a tissue and then throw it in the garbage after each use, or cough or sneeze into your elbow).
- Routine disinfection of shared items and frequently touched surfaces.
- Staying home when sick or experiencing any symptoms of illness.
- Maintaining adequate ventilation and air filtration of shared indoor spaces.
Control Measures for Novel or Variant Viruses
Control measures associated with novel or variant viruses are based on the severity and incidence of the specific virus. Some novel viruses are so mild, or rare, they may go undetected, while others are more contagious or severe. Since new viruses have no historical context, public health guidance evolves as case numbers increase and patterns are identified. That being said, historical pandemic responses have provided a baseline set of evidence-based practices to create a framework for pandemic response planning in the school setting.
Control measures are incremental and based on the current situation. The current situation will be defined by the public health officials and will be based on the severity, incidence, and prevalence in the school setting. Level based responses will then be identified - these are generally defined as using a mild, moderate, and severe category, or for the purposes of this document, level 1, 2, and 3.
When cases of novel viruses are identified globally
When a novel disease is identified, it is the due diligence of school health services personnel and school administration to follow trends. When a novel strain is identified, routine prevention and exclusion measures should continue. In cases where student or staff travel is restricted secondary to pandemic events, it is the staff and parent/guardian’s responsibility to communicate this restriction to the school. The school/district should create a plan to continue to provide education and other services where feasible to students who are unable to attend school in the usual way due to travel restrictions.
When cases of novel viruses are identified regionally or nationally
When a novel disease is identified in the U.S., it is important to identify the geographic spread and maintain awareness of specific public health messaging and direction. The Centers for Disease Control and Prevention (CDC) will have current national guidance. When novel viruses emerge in our state, the Oregon Health Authority (OHA) will provide regional guidance. OHA will have an alert for pandemic-specific content that can be subscribed to for updates. An individual within the district should subscribe to this alert to keep the district updated. If the region impacted is in Multnomah County, the Local Public Health Authority (LPHA) will provide school-centered communication and will potentially host conference calls. When cases are identified in the local region, the Multnomah County Health Department (MCHD) will work with the MESD Nurse Consultant, who will liaise with each component school district, and take part in a response team composed of School Health Services staff and district or individual school leaders, as appropriate. Response teams should be composed of individuals who can fulfill roles with expertise in district policy and administration, clinical information, human resources, building-level management, risk management, and facilities to meet the general structure of Incident Command. The response team should hold regular meetings.
| Personal | Community | Environmental | Communication |
|
|
|
|
When cases of novel viruses are identified in the community
When novel viruses are identified in the community, but not in students or staff, the district will defer to local public health guidance. Public health guidance will likely occur when the overall incidence in the community is increasing (despite the proximity to the school). It is important to note that the school district can only apply controls around the school setting and school-sponsored events and activities. The school district cannot advise control measures around private clubs, organizations, or faith based communities. Each of these congregate settings are responsible for following local public health guidance as well.
When local transmission is detected, planning for cancellation of events and potential for dismissal and academic-continuity should be prioritized. Plans for potential prolonged staff absences should be prioritized, as well.
| Personal | Community | Environmental | Communication |
|
|
|
|
When cases of novel viruses are identified in the school setting
When novel viruses are identified in the school setting, and the incidence is low, the LPHA will provide a direct report to the MESD Nurse Consultant on the diagnosed case. Likewise, the LPHA may impose restrictions on identified close contacts. However, it is important to note that if the incidence is high, the LPHA may not have the capacity to contact-trace and impose individual restrictions. As a result, the LPHA may create public statements that the school district should reiterate. If the school receives a report of a confirmed case, they should immediately contact the MESD Nurse Consultant who will work with the school nurse and building administrator to gather any additional information to assist the health department with contact tracing and advise isolation and quarantine per established protocols
| Personal | Community | Environmental | Communication |
|
|
|
|
Special Considerations
Special Considerations
Employee Sick Leave
Administration and human resources should work together with their legal advisor to determine the need to temporarily revise or flex sick leave to accommodate any public health guidance in regard to lost work. Prolonged exclusion may occur with individuals who are close contacts to a confirmed case, who are identified as suspect cases or who suffer from severe or prolonged illness.
School Closures
If school closure is ordered by the state, the district will abide by the executive order. If a closure is advised by the LPHA, consultation should occur between legal, union, and district administration to ensure processes are consistent with legal preparedness processes.
Immunocompromised Students
Students with immunocompromising health conditions and treatments may require exclusion from school outside of public health guidance. These students should provide documentation from their provider. The change in placement should be accommodated, as appropriate, under the Individuals with Disabilities Education Act (IDEA) and Free Appropriate Public Education (FAPE).
Glossary & References
Glossary of Terms
Glossary of Terms
Administrative controls: Measures used in conjunction with engineering controls that eliminate or reduce a hazard by following established safe work practices and procedures for accomplishing a task safely.
Airborne precautions: Precautions that are utilized to protect against airborne transmission of infectious agents. Diseases requiring airborne precautions include, but are not limited to: Measles, Severe Acute Respiratory Syndrome (SARS), Varicella (chickenpox), and Mycobacterium tuberculosis.
Antibody: A protein produced as an immune response against a specific antigen.
Antigen: A substance that produces an immune response.
Bacteria: Microscopic living organisms. Some bacteria are beneficial, some are harmless, and some can be pathogenic (cause disease).
Biohazard Label: Legend (usually red or orange in color) to identify blood, regulated waste, or other potentially infectious materials (OPIM).
Biological Hazard: Any viable infectious agent that presents a potential risk to human health.
Bloodborne Pathogens: Microorganisms that can cause diseases, such as human immunodeficiency virus (HIV), hepatitis c virus (HCV), and hepatitis B virus (HBV), which are spread through contact with infected blood.
Cohort: A stable group of individuals who spend an extended period of their day in the same space together. In schools, this is likely a classroom, athletic team, before or after school group, bus route, etc. To reduce potential spread of communicable diseases in schools, cohorts should be kept as small as feasible.
Communicable Disease: Illness that spreads from one person to another through contact with the infected person or their bodily fluids, or through contaminated food/water or disease vectors, such as mosquitos or rodents.
Contact Tracing: Public health practice that identifies and notifies individuals who have been exposed to an infectious disease.
Contaminated Waste: Items or surfaces with the presence or reasonably-anticipated presence of blood or OPIMs. These are items that are contaminated with body fluids, but with the capacity to absorb and contain those fluids so that they will not pool or drip. Examples of contaminated waste are diapers, sanitary pads, bandages, minor dressings from wounds or first aid treatment, and PPE. Contaminated items do not need to be placed in a regulated waste container unless they are not able to contain the fluid and there is the possibility that they will allow dripping or pooling of the fluid within the container.
Decontamination: The use of physical or chemical means to remove, inactivate, or destroy the bloodborne pathogens on the surface or item to the point where they are no longer capable of transmitting infectious particles. The surface or item is rendered safe for handling, use or disposal.
Droplet precautions: Preventive methods used for diseases or germs that are spread in tiny droplets caused by coughing and sneezing (examples: pneumonia, influenza, whooping cough, bacterial meningitis).
Engineering Controls: Adjustments to the environment or to processes that eliminate or reduce exposure to hazard (for example, improving the ventilation system in a building).
Epidemic: A disease affecting a large number of people in a community or region.
Exclusion: Preventing someone from entering a place or participating in an activity.
Exposure Incident: A mouth, eye, nose, (mucous membrane), non-intact skin, or parenteral contact with blood or other potentially infectious materials that results from the performance of an employee’s duties.
Immunocompromised: Having a weakened immune system, which limits the body’s ability to fight disease, and therefore cannot respond normally to an infectious agent.
Isolation: Separating symptomatic and infected individuals from the healthy population. A method of controlling the spread of a disease.
Medical Wastes/Infectious Wastes: Blood, blood products, bodily fluids, any waste from human and animal tissues; tissue and cell cultures; human or animal body parts.
Novel: New or previously unidentified, as in, novel coronavirus.
Other Potentially Infectious Materials (OPIM): Human bodily fluid or tissue (other than blood) that can harbor or spread bloodborne pathogens, including but not limited to: saliva, cerebrospinal fluid, semen, vaginal secretions.
Pandemic: An epidemic that spreads across countries or continents.
Parenteral: Piercing the skin-barrier or mucous membranes through such events as needle sticks, human bites, cuts, and abrasions.
Pathogen: A microorganism that can cause disease.
Personal Protective Equipment (PPE): Items used when exposure to hazards cannot be engineered completely out of normal operations and when safe work practices and administrative controls cannot provide additional protection from exposure to infectious or hazardous conditions in a sufficient manner. PPE includes such items as: gloves, gowns, face shields, bite guards, and masks.
Quarantine: Separates and restricts the movement of people who were exposed to a contagious disease to monitor for any symptoms of illness.
Regulated Waste: Liquid or semi-liquid blood or other potentially infectious materials; contaminated items that would release blood or other potentially infectious materials in a liquid or semi-liquid state if compressed; items that are caked with dried blood or other potentially infectious materials and are capable of releasing these materials during handling, including contaminated sharps; and pathological and microbial wastes containing blood or other potentially infectious materials.
Restrictable Diseases: Diseases that require exclusion from work, school and/or childcare facilities for the protection of public health.
Sanitize: Reduce contaminants (viruses, bacteria) on an object or surface.
Seasonal Illness: Illnesses whose occurrence appears to be associated with environmental factors (temperature and humidity changes). For example, colds, and other upper respiratory illnesses are more common during the winter months when people are indoors more often.
Sharps: Any devices that can be used to cut or puncture skin. Examples include: needles, syringes, and lancets (used for checking blood sugar). Sharps must be disposed of in an approved container, to avoid bloodborne pathogen exposure.
Standard Precautions: A set of infection control practices used to prevent transmission of diseases that can be acquired by contact with blood, body fluids, non-intact skin (including rashes), and mucous membranes. These measures are to be used when providing care to all individuals, whether or not they appear infectious or symptomatic.
Surveillance: Collecting and analyzing data related to a disease in order to implement and evaluate control measures.
Transmission: How a disease spreads. There are four modes of transmission:
- Direct—physical contact with infected host or vector
- Indirect—contact with infected fluids or tissues
- Droplet—contact with respiratory particles sprayed into the air (sneezed or coughed)
- Airborne—dried droplets that can remain suspended in the air for long periods of time (e.g., tuberculosis)
Universal Precautions: Preventing exposure to bloodborne pathogens by assuming all blood and bodily fluids to be potentially infectious, and taking appropriate protective measures.
Vaccine: A preparation that is used to stimulate the immune system to produce antibodies to reduce the likelihood of contracting the disease and/or suffer severe disease, including that which results in hospitalization or death.
Vaccinated, fully: The status of having received all recommended vaccine doses in a series at the appropriate age and/or intervals for a specific disease.
Variant: A difference in the DNA sequence, a mutation. Viruses can change and mutate, and these variant forms can be intractable to established vaccines and treatments.
Vector: A carrier of a pathogen that can transmit the pathogen to a living host. Mosquitoes, fleas, ticks, and rodents are examples of vectors.
Work practice controls: Measures intended to reduce the likelihood of exposure by changing the way a task is performed. They include appropriate procedures for handwashing, sharps disposal, lab specimen handling, laundry handling, contaminated material cleaning (OSHA, 2019b), and prohibiting two-handed manipulation of contaminated sharps.
References
References
BC Center for Disease Control (BCDC) (2021) A quick Guide to Common Childhood Diseases. Retrieved from http://www.bccdc.ca/schools/Documents/EN_Guide_Childhood_Diseases.pdf
Centers for Disease Control and Prevention. (2024). Influenza. Retrieved from https://www.cdc.gov/flu/about/index.html
CDC (2024) Preventing Spread of Respiratory Viruses When You’re Sick. Retrieved from https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick...
CDC (2024) When and how to wash your hands. https://www.cdc.gov/handwashing/when-how-handwashing.html
CDC (2023) Variant Influenza Viruses: Background and CDC Risk Assessment and Reporting. Retrieved from https://www.cdc.gov/swine-flu/variant-flu-in-humans/risk-and-reporting.h... dc.gov/flu/swineflu/variant.htm
Federal Emergency Management Agency (FEMA) (2023) Non-Pharmaceutical Interventions. Retrieved from https://www.fema.gov/cbrn-tools/key-planning-factors-bio/kpf-3/1
Montana Department of Public Health and Human Services (MDPHHS) (2023) Communicable Disease: A guide forSchools in Montana. Retrieved from https://dphhs.mt.gov/assets/publichealth/CDEpi/DiseaseReporting/MasterFI...
National Resource Center for Health and Safety in Child Care and Early Education (NRC). (2020). Environmental Health in Early Care and Education. Retrieved from https://nrckids.org/CFOC/Environmental_Health
Occupational Safety and Health Administration (2019). Occupational Safety and Health Standards. Retrieved from https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1030
Oregon Department of Education (2024) Communicable Disease Guidance for Schools. Retrieved from https://www.oregon.gov/ode/students-and-family/healthsafety/Documents/Up...
Victoria State Government. (2023). Managing spills of blood and body fluids and substances. Retrieved from https://www.health.vic.gov.au/infectious-diseases/managing-spills-of-blo...
Virginia Department of Health (2011) FAQ Respiratory Hygiene and Cough Etiquette. Retrieved from https://www.vdh.virginia.gov/content/uploads/sites/3/2016/01/Respiratory...
Weatherspoon, D. (2019) Acute Viral Respiratory Infections. Retrieved from https://www.healthline.com/health/acute-respiratory-disease
World Health Organization (WHO) (2019) Non-pharmaceutical Public Health Measures for Mitigating the Risk and Impact of Epidemic and Pandemic Influenza. Retrieved from https://iris.who.int/bitstream/handle/10665/329438/9789241516839-eng.pdf
Communicable Disease Management Tools
Symptom Based Exclusion Chart
Parents, students, and staff should be taught to not come to school if experiencing any of the following:
|
EXCLUSION CRITERIA |
EXCLUSION ACTION |
|
Fever: temperature of 100 .4°F (38°C) or greater |
|
| New cough illness |
|
| New difficulty breathing |
|
| Diarrhea: Three (3) loose or watery stools in a day OR not able to control bowel movements |
|
| Vomiting: Two (2) or more episodes that are unexplained |
|
| Headache with stiff neck and fever |
|
|
Skin rash or open sores |
|
| Red eyes with colored drainage |
|
|
Jaundice: new yellow color in eyes or skin |
|
|
Acting differently without a reason: unusually sleepy, grumpy, or confused |
|
|
Major health event, like an illness lasting two (2) or more weeks OR a hospital stay, OR health condition requires more care than school staff can safely provide |
|
Communicable Disease Sheet (CDS)
Schools may track reports of communicable diseases in their population at any given time. This Communicable Disease Sheet is an example of a tracking sheet that can be shared between front office staff taking phone calls from parents reporting student absences due to communicable disease.
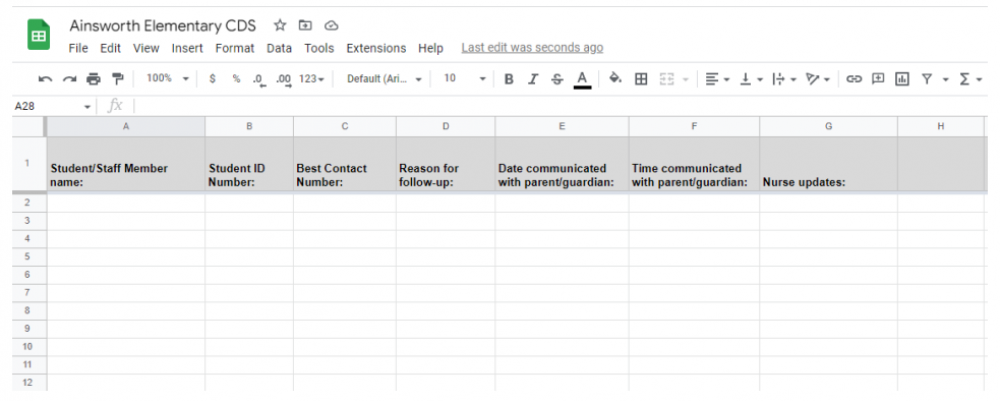
Donning & Doffing (Applying & Removing) PPE
Donning (applying) PPE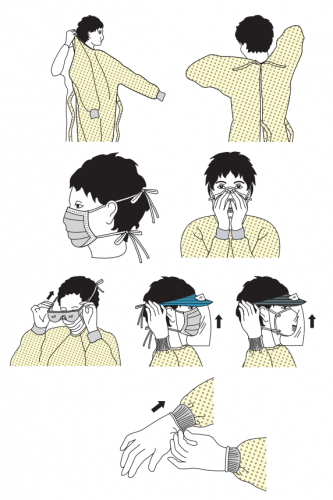
- Perform appropriate hand hygiene.
- Determine appropriate PPE to be worn depending on duties being performed
-
Put on gown, if applicable.
- Fully cover your torso from your neck to knees and your arms to the end of your wrists, then tie at the back.
- The gown should be large enough to allow unrestricted movement without gaping.
- Fasten at the back of the neck and waist.
-
Put on medical grade mask , if applicable
- Fit the flexible band to the nose bridge.
- Fit mask snug to face and below the chin.
- Put on protective eyewear or face shield, if applicable. o Place over eyes/face and adjust to fit.
- Put on gloves. o Extend the gloves to cover the wrist of the gown.
Donning must be performed in the correct order to prevent infection transmission.
Doffing (removing) PPE
Following a correct doffing procedure is especially crucial in the control and prevention of infection. It is the most important step of preventing infection transmission. The doffing of PPE should protect your clothing, skin and mucous membranes from contamination.
Remember that all PPE is contaminated after use. Perform hand hygiene immediately after each step of doffing. 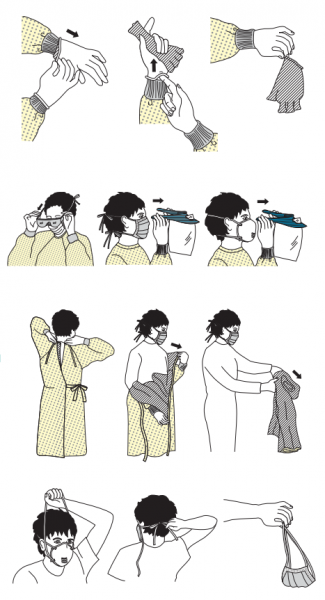
If you are in the isolation space, your gloves and gown (if applicable) should be removed before exiting the room.
-
Remove gloves
- Using one hand, grasp the palm of the other hand and peel off the first glove
- Hold the removed glove in the gloved hand
- Slide fingers of the ungloved hand under the remaining glove at the wrist and peel it off over the first glove
- Discard gloves in a waste container
- Perform hand hygiene appropriately
-
Remove goggles/face shield, if applicable
- Remove from the back of the head by lifting headband or earpiece.
- If reusable, place in the designated reprocessing receptacle. If not, discard in waste container.
-
Remove gown
- Unfasten the ties, ensuring the sleeves do not make contact with your body
- Pull the gown away from the neck and shoulders, touching the inside only
- Turn the gown inside out
- Fold or roll the gown into a bundle and discard in the waste container
- Perform hand hygiene
- If applicable, exit isolation space
- Perform hand hygiene
-
Remove mask
- Grasp the elastic ties looped around the ears and remove without touching the front of the mask
- Discard in the waste container
- Immediately perform hand hygiene
Body Fluid Exposure Protocol
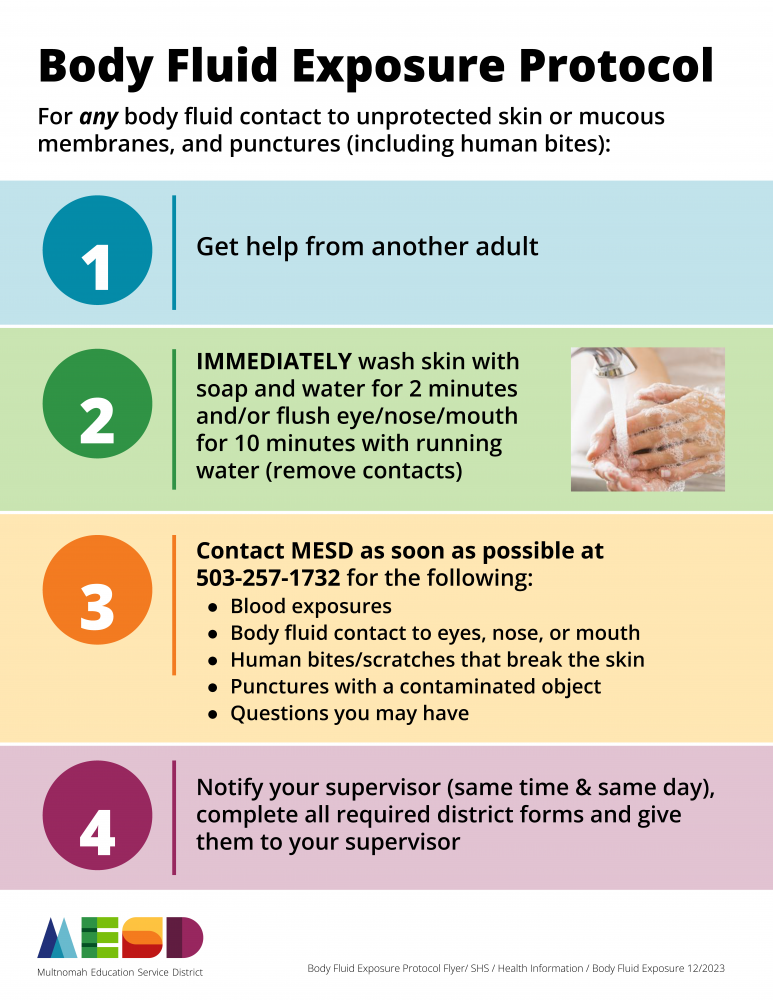
Opioid Overdose Information
Opioid Overdose Information
Our school holds student well being at the heart of the work that we do. We are sharing concerns about fentanyl and opioid drugs. These drugs are harming people in our community. We hope this information will help protect students. This following is valuable information including guidance on how to respond to an overdose and resource links.
Teen drug use has been decreasing over time. However, data shows that there has been an increase in overdoses, mainly due to illicit fentanyl in the drug market (NIDA, 2023). It is crucial to educate students and young people about substance use risks, including the potential of fentanyl in illicit pills and other substances. It is also important to raise awareness about opioid antagonists (such as naloxone).
What is an opioid? Opioids come from the opium poppy plant and include drugs like morphine, oxycodone, dilaudid, heroin, and fentanyl. They attach to receptors to block pain and increase pleasure. Overdose is a common risk associated with opioids and can be intentional or accidental. Fentanyl is a powerful opioid: a dose as small as a few grains of sand can make a person stop breathing within minutes.
Why do people use opioids? Opioids may be prescribed as pain medicine. Some young people try drugs because they are curious. Some people use drugs to avoid feeling difficult emotions. Opioids are addictive.
What is an opioid antagonist? Opioid antagonists are medications (naloxone is the most commonly known opioid antagonist) that can be delivered by a nasal spray or injection to quickly restore normal breathing for a person whose breathing has slowed down or stopped because of an overdose of fentanyl, prescription opioids or heroin. Naloxone onset occurs within 2-3 minutes and can last for 30-90 minutes. Sometimes a second dose of naloxone is necessary if symptoms of overdose return. Naloxone may be administered in emergency overdose situations and is safe for the person receiving the medication.
What can you do? Please talk about the dangers of fentanyl and availability of opioid agonists with your students and others you care about. Consider having naloxone available in your home for the quickest response during a medical emergency. Learn more about how to get naloxone and how to use it here: Opioid Overdose Reversal Medications
What is your school district doing? Reynolds School District provides comprehensive drug and alcohol education aligned with the 2023 Oregon Health Education Standards. In addition, we care deeply about the health and safety of every student in our school community. In alignment with school district policy, all schools will stock naloxone and necessary medical supplies. Staff may administer naloxone to any person suspected of experiencing an opioid overdose. Anytime naloxone is administered school staff will call 911 and notify the student’s parents or guardian.
In alignment with school district policy, some schools will stock naloxone and necessary medical supplies at the following schools: H.B. Lee Middle School, Reynolds Middle School, Walt Morey Middle School, Reynolds High School, and Reynolds Learning Academy. Staff may administer naloxone to any person suspected of experiencing an opioid overdose. Anytime naloxone is administered, school staff will call 911 and notify the student’s parent or guardian.
We know these conversations can be hard. The best person to contact should you have questions is:
Dr. Holly Altiero
Student Services Program Administrator
haltiero@rsd7.net